How Phalloplasty Is Staged
Just as there are a number of different Phalloplasty procedures, there are also several different ways that Phalloplasty surgery can be staged over time. Understanding the how and why behind the different ways of staging Phalloplasty is key to selecting a surgeon and planning for your surgery. This article examines the different approaches Phalloplasty surgeons have for how the surgery is staged.
1 Stage Tube-Within-a-Tube
The most commonly understood way of staging Phalloplasty surgery is the 1-stage tube-within-a-tube design of the Radial Forearm Flap Phalloplasty (RFF). Developed in the early '80s, the primary advance of this design was the creation of a vascularized urethra incorporated into the phallus (a tube-within-a-tube) in one stage. Previous efforts created the urethra with a skin graft or prefabricated with a multistaged tubed pedicle flap, which invariably led to increased urethral complications.1
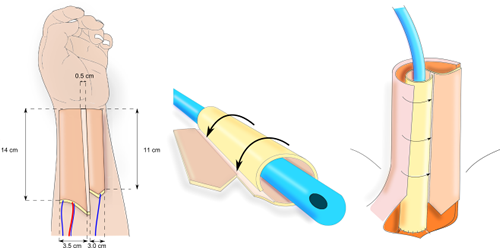
This approach typically includes vaginectomy, creation of the phallus with a full urethra, scrotoplasty and glansplasty in Stage 1. The second stage surgery usually occurs anywhere from 6 to 12 months later and includes insertion of testicular and erectile prosthetics. The "1-Stage" name of this approach refers to creation of phallus and full urethra in a single stage. While additional stages are sometimes required for aesthetic improvements (liposuction, fat grafting, mons resection, etc.) or functional repairs, a benefit of this approach is that the surgery can often be completed in just two operative events. In terms of financing and scheduling surgery, this is a major advantage for patients.
Some surgeons offer Integra to their patients to improve the appearance of the donor site. Integra helps close the forearm wound faster and with less contraction. If Integra is used, an additional stage is added 2-3 weeks following Stage 1 to replace the Integra with a skin graft. (For more details, see How Integra Works.)
Staged ALT Phalloplasty
While 1 Stage Tube-Within-a-Tube ALT Phalloplasty is appropriate in the right patient, some surgeons offer ALT Phalloplasty with additional stages to enable urethroplasty or to improve vascularity. For example, if the ALT flap has too much subcutaneous fat, the tube-within-a-tube design is not possible. If standing-to-pee is desired, an additional stage can be added to incorporate non-vascularized urethroplasty, using a buccal mucosa graft, vaginal mucosa graft (if available) or skin grafts, though non-vascularized urethroplasty reportedly has a high rate of fistula and stricture complications.
 Another
multi-stage approach for ALT Phalloplasty is the Delayed
ALT Flap practiced by Dr.
Curtis Crane. Designed to improve flap
vascularity, Delayed ALT Flap involves elevating the ALT flap,
severing the secondary blood supply while the main blood supply is
preserved, and then putting the flap back in place in Stage 1.
(Vaginectomy may or may not be included in Stage 1.) Creation of
the phallus takes place in Stage 2, after the vascularity of the
flap has improved. Delayed ALT Flap adds an additional stage to
the surgery but allows patients who are borderline candidates for
ALT, or who have blood supply issues in the ALT flap, to still use
the ALT donor site.
Another
multi-stage approach for ALT Phalloplasty is the Delayed
ALT Flap practiced by Dr.
Curtis Crane. Designed to improve flap
vascularity, Delayed ALT Flap involves elevating the ALT flap,
severing the secondary blood supply while the main blood supply is
preserved, and then putting the flap back in place in Stage 1.
(Vaginectomy may or may not be included in Stage 1.) Creation of
the phallus takes place in Stage 2, after the vascularity of the
flap has improved. Delayed ALT Flap adds an additional stage to
the surgery but allows patients who are borderline candidates for
ALT, or who have blood supply issues in the ALT flap, to still use
the ALT donor site.
Even when Tube-Within-a-Tube ALT Phalloplasty is possible, glansplasty is not done in Stage 1 due to vascular concerns.
Primary and Secondary Urethroplasty
In an effort to reduce urethral complications, there is a growing trend of surgeons performing urethral reconstruction over two stages, and this can be done in a couple of different ways. For example, what is essentially a Metoidioplasty can be performed in Stage 1, along with vaginectomy, extending the native urethra by just a few inches initially, then extending it to the tip of the phallus in Stage 2.2 A similar approach involves creation of the phallus with a urethra in Stage 1, and connection to the native urethra and vaginectomy taking place in Stage 2 about 6 months later.
Staging Phalloplasty in this way can reduce the incidence of multiple concurrent complications, improving quality of life for the post-operative patient. Staging Phalloplasty also offers the opportunity for patients to carefully consider additional surgeries—such as vaginectomy and burying the clitoris.
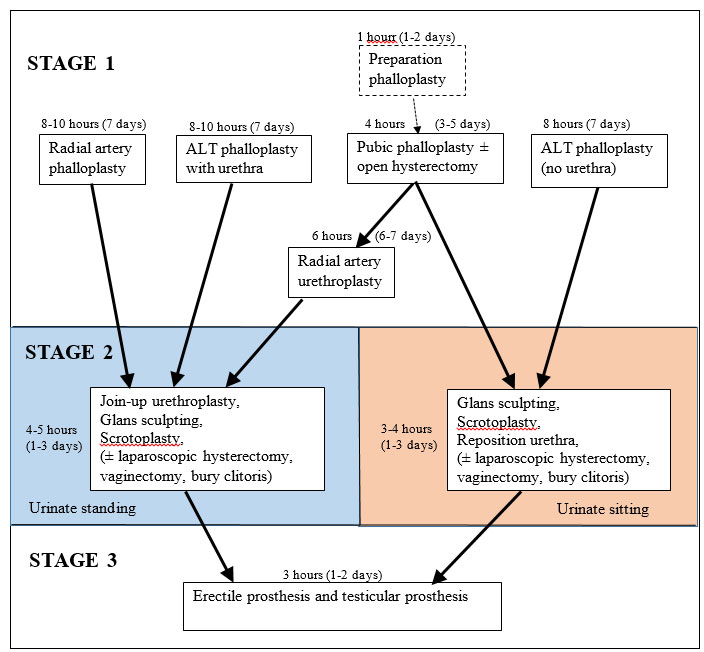
How the surgeons at the St. Peter's Andrology Centre in London stage Phalloplasty. Source: andrology.co.uk
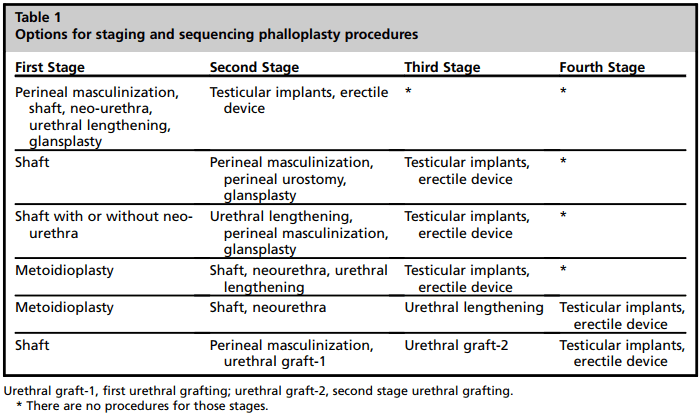
Source: Staging in Phalloplasty. Danker et al.
Prefabrication and Prelamination of the Urethra
Additionally, there are surgeons who offer prefabrication or prelamination of the urethra using either a full or split thickness skin graft, which adds a stage before creation of the phallus. However, some surgeons believe the indications for urethral reconstruction in this manner should be limited to cases for which no other option is suitable.3
Prelamination with mucosal grafts also has been reported as a possible method of reducing urethral complications but more investigation is needed.4 Dr. Christopher Salgado uses the prelamination technique with mucosal grafts from the inside of the cheeks and/or vagina, wrapping them around a catheter and placing the structure under an elevated forearm flap.5 This is left in place until the tissues are transferred to the groin in stage 2.
WATCH: Patient of Dr. Salgado's explains aftercare for prelaminated urethra.
As more research is done into ways of improving Phalloplasty outcomes, the different ways of staging Phalloplasty will likely develop as well. As it stands, Phalloplasty surgeons offer a number of different options for staging Phalloplasty, including approaches where either creation of the the phallus or the completion of the urethra are delayed. For patients, the staging of Phalloplasty is another important consideration when choosing a surgeon and a surgical technique.
Related Studies
Staged
Phalloplasty by Metoidioplasty First Does Not Appear to Lower
Complication Rates
Mieke Waterschoot, Piet Hoebeke, Wesley Verla, Anne-Françoise
Spinoit, Stan Monstrey, Marlon Buncamper and Nicolaas Lumen. 7 Jun
2023. Transgender Health.
Some patients opt to undergo staged phalloplasty by metoidioplasty
first (SPMF). The aim of this study was to evaluate whether SPMF
is associated with less surgical complications compared with
immediate phalloplasty (IP). In our cohort, complications were not
reduced by SPMF. In case metoidioplasty is considered as a step
toward phalloplasty, separate morbidity of metoidioplasty must be
taken into account.
The
Montréal Classification of urethral lengthening for phalloplasty
in transmasculine patients-surgical techniques and urethral
complications.
Bonapace-Potvin M, Lorange E, Ma X, Medor MC, Bensimon É, Brassard
P, Bélanger M. Int J Transgender Health. 2022 Aug
9;24(4):461-468.
In this study, post-operative urological complications for
immediate anastomosis versus two-stage anastomosis were reported
in 77.7% and 18.2% of patients, respectively. Over the last few
years, the Montreal team has shifted away from single-stage
anastomosis and has adopted a two-stage anastomosis technique.
Neourethra
Creation in Gender Phalloplasty: Differences in Techniques and
Staging
Berli JU, Monstrey S, Safa B, Chen
M. Plast Reconstr Surg. 2021 May
1;147(5):801e-811e.
Neourethra reconstruction is the most challenging aspect of
phalloplasty, with widely varying techniques and staging
between providers. In this expert opinion article, the authors
strive to give an overview of the principles behind, and a
detailed explanation of, the technical details of creating the
penile and bulbar urethra during phalloplasty. The authors focus
on the three most common strategies: single-stage phalloplasty;
two-stage phalloplasty with a metoidioplasty-first approach; and
two-stage phalloplasty with a phalloplasty-first (Big Ben method)
approach. It is not the authors' intent to establish the "best" or
"only" way, but rather to compile different options with their
respective pros and cons.
Single
versus two-stage phalloplasty for transgender female-to-male
patients: a systematic review of the literature. [FULL
TEXT]
Huayllani MT, Boczar D, Saleem HY, Cinotto G, Avila FR, Manrique
OJ, Ciudad P, Rinker BD, Forte AJ. Ann Transl Med.
2021 Apr;9(7):608.
In this study, two-stage phalloplasty had greater rate of
complications such as urethrocutaneous fistulas and total/partial
flap necrosis when compared to a single-stage phalloplasty.
References:
1. Gottlieb LJ. Radial Forearm. Clin Plast Surg. 2018 Jul;45(3):391-398.
2. Gottlieb.
3. Monstrey SJ, D'Arpa S, Colebunders B, Lumen N, Hoebeke P. Anterolateral Thigh Flap Phalloplasty in Gender Affirmation: Medical and Surgical Perspectives (Thieme, Dec 1, 2016.)
4. Salgado CJ, Fein LA, Chim J, Medina CA, Demaso S, Gomez C. Prelamination of Neourethra with Uterine Mucosa in Radial Forearm Osteocutaneous Free Flap Phalloplasty in the Female-to-Male Transgender Patient. Case Reports in Urology, Volume 2016.
5. Christopher J. Salgado MD, Ajani Nugent MD, Josef Hadeed MD,
Maria Lalama BS, Jorge Rey MD & Carlos Medina MD. Two-Stage Prelaminated Mucosal Neourethra
Radial Forearm Flap Phalloplasty for Transgender Men [FULL
TEXT]
Global Journal of Medical Research: I Surgeries and
Cardiovascular System, Volume 21, Issue 1, 2021.
6. Sara Danker, Nick Esmonde, Jens Urs Berli. Staging in Phalloplasty. Urol Clin North Am. 2019 Nov;46(4):581-590.
Last updated: 01/25/24
